Healthcare has certainly evolved in the past few years. According to 2019 Definitive Healthcare data, only about 33% of inpatient hospitals and 45% of outpatient facilities offered telehealth services to their patients. Now, about 75% of U.S. hospitals are using telemedicine systems—a 42% increase from 2019 usage.
This explosion is, of course, driven by the COVID-19 pandemic. Telemedicine has proven to be a key revenue driver and delivery platform that gave providers reach and connection with their patients when in-person care was not possible. But is this sustainable moving forward? Will we return to traditional brick-and-mortar facilities for healthcare? Or, can virtual and brick-and-mortar care coexist?
In this new era of healthcare with a large focus on patient experience and consumerism, providers and organizations need to remain flexible with how they are engaged. Virtual care is not limited to just teleconferencing or video calls. It extends to wearables, monitors and mobile apps. Telehealth, which initially was developed to provide basic care to rural and underserved patients, has evolved into an approach that nearly every healthcare organization provides, regardless of location. Increasing emphases on patient satisfaction, providing efficient and quality care, and minimizing costs have also led to higher telehealth implementation.
In 2021, digital health startups raised $29.1 billion. This trend slowed a little in the first quarter of 2022 to $6 billion, compared to $7.3 billion raised in the fourth quarter of 2021, according to Rock Health. With all this money and capital moving toward solutions that allow patients to be seen on their own time and in their own homes, the brick-and-mortar healthcare organization could face some challenges. However, there are still many barriers that prevent telehealth solutions from completely taking over the industry.
Telehealth is convenient because the care can be synchronous (communication in real time) and asynchronous (data, images or messages are recorded to share with the doctor later), and provide remote patient monitoring (blood sugar levels or weight sent to the healthcare provider), but not all consumers are convinced this platform is the way of healthcare. In addition, current policies may not completely support a telehealth platform. As of February 2022, for reimbursement for live video services under Medicaid, only 19 states required private insurances to implement payment parity, four states had payment parity policies with caveats and 27 states had no payment parity. These inconsistencies across states make it difficult to adopt telehealth, enforce mandates and impact pricing.
Additionally, some consumers of telehealth solutions are wary of security within the virtual platform and being misdiagnosed. There is also concern around cost because if something is not captured or explained well during a telehealth visit, the patient may need to be seen in person, which would add costs. Many patients were thrilled about telehealth visits during the pandemic because it helped keep them away from other potentially sick people, but some possible preventive conditions may not have been addressed during that time or treated as well as they would have been if patients had in-person visits. Going forward, brick-and-mortar in-person visits may be the preferred method for addressing preventive conditions.
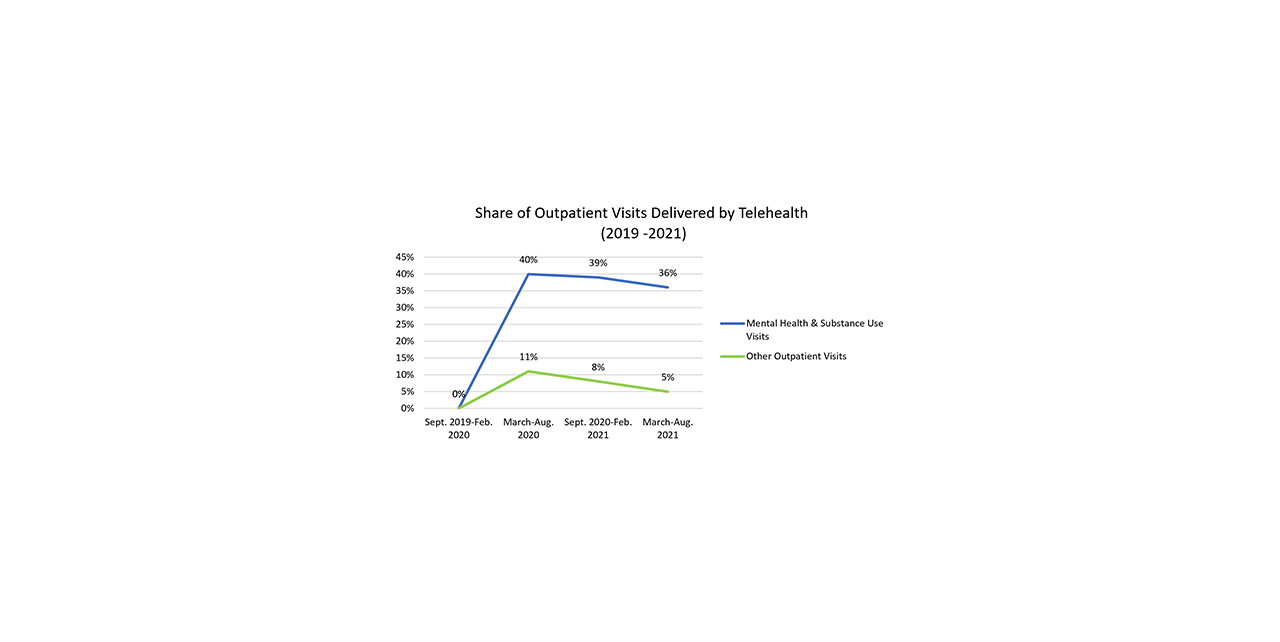
The following chart shows the trend of patients receiving telehealth care for outpatient visits. Telehealth has become very useful for patients with mental health needs, for instance, but it has not captured and met the needs of all care specialties. As more COVID-19 restrictions are relaxed, the data shows that patients and providers prefer to have a mix of in-person and virtual visits to improve the patient experience and increase overall care. As more technology and private organizations enter the industry, patients will have many options for how to receive care. Time will tell, but perhaps a hybrid of telehealth offerings and in-person visits is the ideal approach for healthcare delivery and for providers to remain competitive moving forward.
As of today, it isn't possible to do every type of healthcare visit remotely. Patients still need to go into the office for things like imaging tests and blood work, as well as for diagnoses that require a more hands-on approach. The new era of healthcare is likely a place where a combination of both in-person and virtual care is needed as hospitals and healthcare organizations expand their engagement with patients in bettering the experience and lowering the cost of care.
Michael Haas is a health care senior analyst with RSM US LLP.